20.12.2019
The first article presents a review of current data on the applications of photobiomodulation (PBM) in the field of oral and maxillofacial surgery (OMFS), to guide future research. The second systematic review aimed to comprehensively review all available documents regarding photobiomodulation therapy (PBMT) application in temporomandibular disorder (TMD) patients and to suggest an evidence-based protocol for therapeutic PBM administration for these patients.
ABSTRACTS
Photobiomodulation in Temporomandibular Disorders
Jan Tunér, DDS,1 Sepanta Hosseinpour, DDS, MPH, PhD,2 and Reza Fekrazad, PhD, DDS3
Objective: This systematic review aimed to comprehensively review all available documents regarding photobiomodulation therapy (PBMT) application in temporomandibular disorder (TMD) patients and to suggest an evidence-based protocol for therapeutic PBM administration for these patients.
Background data: The existence of temporomandibular joint and/or pain and dysfunction in masticatory muscles is characterized in TMDs. PBMT is, due to its impact on biological processes, especially inflammation, considered as an adjuvant treatment modality in TMD cases. Materials and methods: All original articles related to PBMT for TMDs in EMBASE, MEDLINE (NCBI PubMed and PMC), Cochrane library, Scopus, Web of Science, and Google Scholar were reviewed until December 2018.
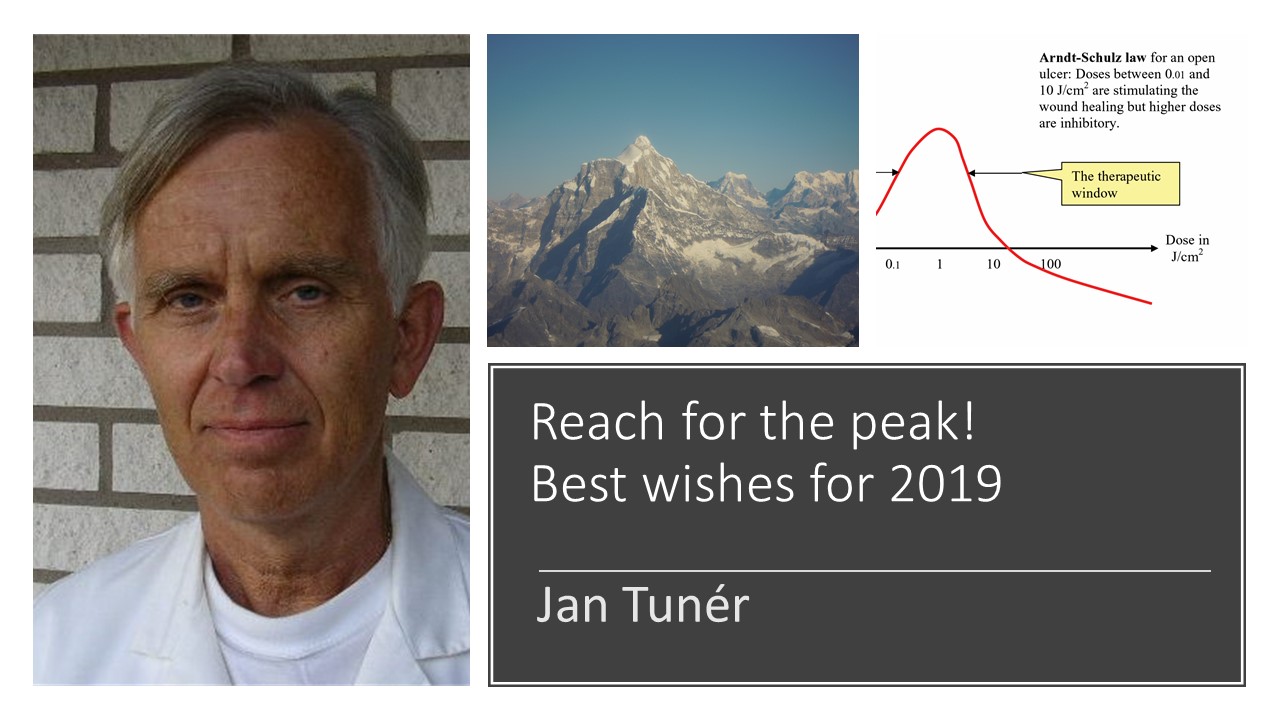
Results: The energy density ranging from 0.75 to 112.5 J/cm2 with 0.9?500mW power was found to be a window protocol for light application. The best results for pain relief and mandibular movement enhancement were reported after application of GaAlAs diode laser, 800?900 nm, 100?500mW, and <10 J/cm2, twice a week for 30 days on trigger points. The session of light applications varied from 1 to 20.
Conclusions: Although most articles showed that PBMT is effective in reducing pain and contributed to functional enhancement in TMD patients, the heterogenic parameters that have been reported in various studies made the standardization of PBMT complicated. However, such evidence-based consensus can be beneficial for both future research and for clinical applications.
Photobiomodulation in Oral Surgery: A Review
Sepanta Hosseinpour, DDS, MPH, PhD Student,1 Jan Tunér, DDS,2 and Reza Fekrazad, DDS, PhD, FLD, FICD3,4
Objective: This article presents a review of current data on the applications of photobiomodulation (PBM) in the field of oral and maxillofacial surgery (OMFS), to guide future research. Background data: Photobiomodulation therapy (PBMT) has been reported to be effective for various postoperative conditions, including pain relief, improvement of mastication, neurosensory recovery, and wound healing. There is a need for identifying the therapeutic irradiation windows for these conditions, based upon the available literature.
Materials and methods: All original articles related to PBM for oral surgery in MEDLINE (NCBI PubMed and PMC), EMBASE, Scopus, Cochrane library, Web of Science, and Google Scholar were reviewed until December 2018.
Results: Forty-six clinical trials were included in this study. These trials were categorized into three different types of PBM applications. After reviewing all these studies, the most effective physical properties for PBM pain reduction after tooth extraction were as follows: wavelength 650?980 nm; power 4?300mW; and energy density 3?85.7 J/cm2. PBMT at 660?910nm with 4?500mW power and 2?480 J/cm2 energy density was effective for decreasing facial swelling. At the same wavelength and power range with 4?106 J/cm2 energy density, PBM was effective for alleviating trismus after tooth extraction.
Conclusions: Most papers suggested that PBM seemed to be effective in reducing pain, swelling, and trismus after third molar tooth extraction, neurosensory and nerve recovery after mandibular ramus osteotomy. The heterogeneity of the standardization regarding the parameters of laser calls for caution in interpretation of these results. However, this evidence-based review regarding the best protocols for OMFS applications can be beneficial for both future research and clinical applications.
Both reviews full text available: Photobiomodulation, Photomedicine, and Laser Surgery